You’re the person patients turn to when their world is falling apart. You sit with them in their darkest moments, hearing stories of trauma, pain, and heartbreak that would break most people. You absorb it all because that’s what you do—you care.
But what happens when you’re the one falling apart? Burnout doesn’t hit you all at once. It creeps in. First, it’s the constant exhaustion, no matter how much you sleep.
Then it’s the emotional numbness—smiling at your patients while feeling like there’s nothing left inside of you. And the worst part? Feeling like you’re failing, even though you’ve been giving everything you have.
Being a PMHNP isn’t just mentally taxing—it’s soul-crushing when no one sees the toll it’s taking. You’re surrounded by people who need you, yet you feel completely alone, carrying a weight that’s slowly breaking you.
But hey! this doesn’t mean you’re weak. It means you’ve been carrying too much stress for too long, and it’s time to set some of that weight down.
In this blog, more than offering burnout prevention tips—we’re acknowledging the very real struggles PMHNPs go through and giving you the tools to take back control of your well-being and avoid burnout.
Understanding burnout
What is burnout?
Burnout is more than just feeling tired after a long day. It’s a state of emotional, mental, and physical exhaustion caused by prolonged stress, overwork, and a lack of balance in life. Imagine feeling hopeless, detached, and cynical about your work and life in general. That’s burnout. It doesn’t discriminate—it can affect anyone, regardless of their profession or position. The parental burnout inventory is a tool used to assess burnout in parents, drawing a parallel to the assessment of burnout in PMHNPs. And for PMHNPs, the consequences can be severe, impacting your mental and physical health, relationships, and overall well-being.
Signs and symptoms of burnout
Burnout manifests differently for everyone, but there are common signs you shouldn’t ignore:
- Chronic fatigue and exhaustion: Feeling tired all the time, even after a full night’s sleep.
- Cynicism and detachment: Becoming increasingly negative or detached from your work and the people around you.
- Reduced productivity andperformance: Struggling to keep up with your workload and noticing a decline in your performance.
- Increased absenteeism and tardiness: Finding it harder to get to work on time or taking more sick days.
- Irritability and mood swings: Experiencing frequent mood swings and irritability.
- Lack of motivation and interest: Losing interest in work and activities you once enjoyed.
- Physical symptoms: Suffering from headaches, stomach problems, and sleep disturbances.
- Difficulty concentrating: Struggling to focus and make decisions.
- Feeling overwhelmed and hopeless: Feeling like you’re drowning in your responsibilities and can’t see a way out.
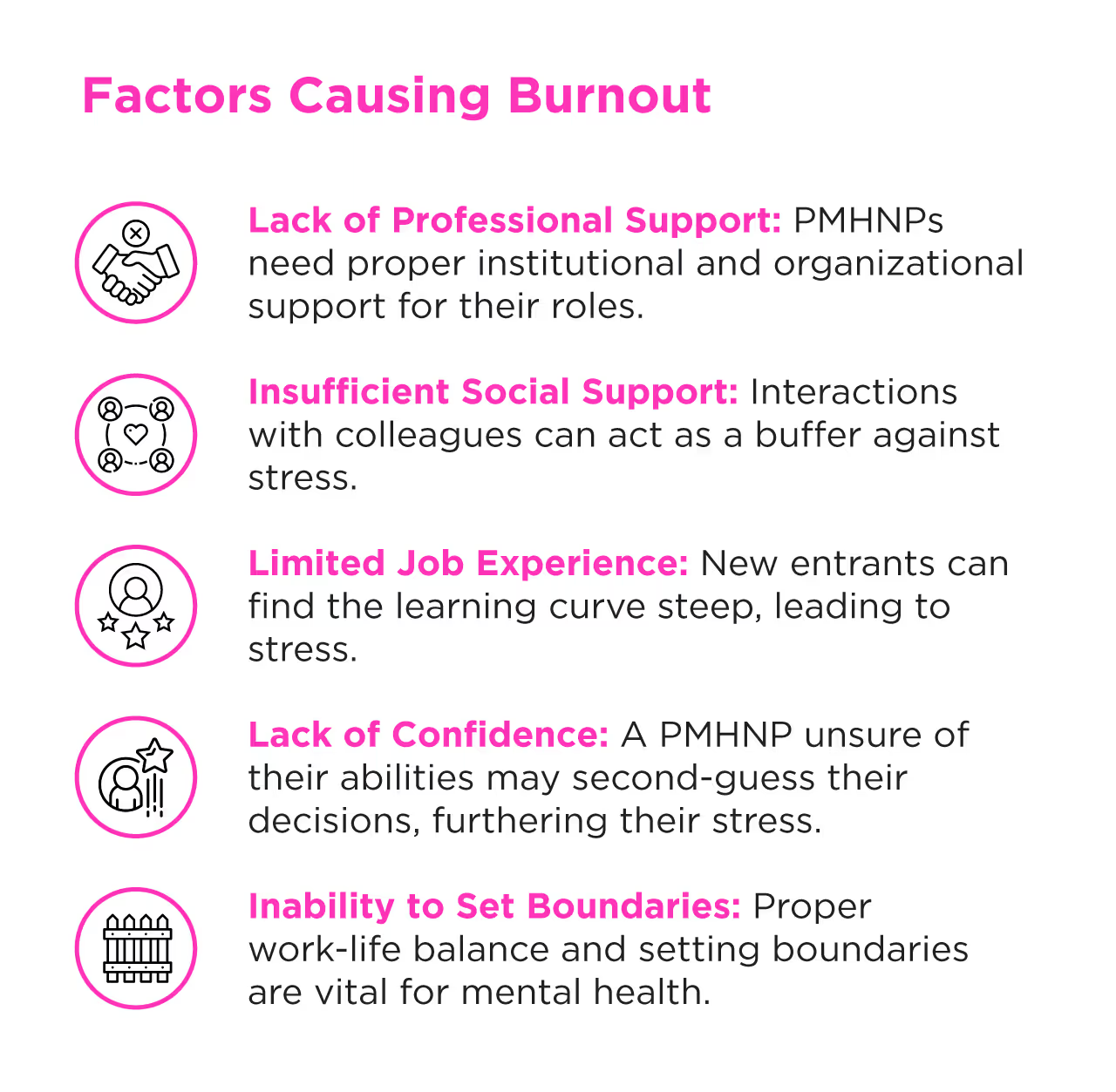
Why PMHNPs are especially vulnerable to burnout?
Let’s call it like it is: being a psychiatric nurse practitioner is hard. Chronic stress is a significant phase in the progression of burnout, where individuals consistently feel tired and experience emotional detachment, leading to social withdrawal and various physical symptoms. Your work isn’t just physically demanding—it’s emotionally draining in ways that few people truly understand. Reducing stress is crucial to enhance well-being and prevent burnout. You’re often dealing with:
1. The emotional exhaustion of the work
You’re not just treating symptoms; you’re diving into the deepest, most complex parts of your patients’ lives. Every day, you absorb stories of trauma, abuse, and despair. Over time, that emotional labor doesn’t just stay at work—it follows you home, leading to emotional exhaustion, a significant psychological consequence of workplace stress, making it hard to recharge.
2. Patient aggression and resistance
Handling patients who are aggressive or resistant to treatment isn’t just challenging—it’s draining. It forces you to constantly adapt, often leaving you second-guessing your decisions or questioning your effectiveness.
3. Systemic pressures and chronic stress
Many PMHNPs are asked to do more with less—more patients, less time; more documentation, fewer resources. Add to that the unrealistic expectations for productivity, leading to too much stress, and it’s no wonder you feel like you’re always falling short.
4. Isolation in the profession
Unlike other specialties, where you might work alongside a team in close collaboration, mental health care can feel isolating. This lack of camaraderie and shared burden often leaves you feeling like you’re carrying everything alone.
5. Personal sacrifices
Let’s not forget the personal sacrifices you make daily. Long hours mean less time for your family, hobbies, and self-care. The imbalance can leave you feeling resentful or like you’re losing parts of yourself outside of work.
While you’re giving everything to your patients, who’s giving to you? The system often doesn’t. Long hours, high patient loads, and the expectation that you’ll “just handle it” pile up until you’re left feeling like you have nothing left to give.
What are some warning signs you shouldn’t ignore?
You’re running on fumes:
You wake up feeling like you didn’t sleep. Getting enough sleep is a critical component of overall well-being and burnout prevention. The idea of getting through another shift feels heavier than ever. What used to come naturally—your compassion, your drive—now feels like a chore.
You’re starting to feel numb:
Patients’ stories don’t hit you the same way anymore. You catch yourself tuning out, or worse, feeling resentful. It’s like you’re building a wall to protect yourself, but it’s also cutting you off from the parts of your work you used to love.
Your body is screaming for help:
Mental exhaustion caused by prolonged stress and overwork can lead to chronic headaches, an upset stomach, and that bone-deep fatigue that no amount of sleep, coffee, or “just powering through” can fix. Your body knows before you do that something’s not right. The stress response can lead to physical symptoms like headaches and stomach problems.
You’re slipping at work:
Focus feels impossible. Deadlines pass. You’re going through the motions, but the pride and satisfaction you used to feel are gone. Everything feels harder than it should.
You’re pulling away from everything:
You procrastinate on tasks you used to tackle head-on. You’re avoiding colleagues, dodging phone calls, and skipping out on things that usually bring you joy because it all feels like too much.
These aren’t just tough days or a stressful week. These are your mind and body waving red flags, asking—no, begging—you to listen. Ignoring them doesn’t make them go away. It just lets burnout tighten its grip.
How to prevent and overcome burnout before it stops you?
It’s not enough to say “practice self-care” and call it a day. Preventing burnout requires a mix of intentional actions and real support. Here’s how you can start:
1. Set boundaries like your life depends on it
When was the last time you really shut off from work? Not just logging out of your email, but actually putting it all down and saying, “I’m done for today”? If you’re struggling to answer, that’s a problem—and it’s one we need to talk about.
Here’s the thing: if you don’t set boundaries, no one will do it for you. Work will take as much as you’re willing to give, and before you know it, there’s nothing left. You’re exhausted, snapping at loved ones, and wondering why you feel so burned out. Boundaries aren’t a luxury—they’re a lifeline.
2. Master your calendar:
Your calendar isn’t just a tool to keep track of patients and meetings—it’s your shield. Block off time for everything. Patient care, admin work, and—this is the big one—time for yourself. And I don’t mean vague “self-care” time. I mean specific, intentional blocks where you step away, recharge, and protect your mental space.
But here’s the kicker: you have to honor those blocks. Treat them like they’re as important as a meeting with your boss. Because guess what? They are. If someone tries to encroach on that time, the answer is simple: “No, I can’t. I have a prior commitment.” That prior commitment is you.
3. Learn to push back without apologizing
Let me guess—you hate saying no. You feel like you’re letting someone down, or maybe you’ve been told that saying yes to everything is part of the job. But here’s the truth: saying no is how you protect yourself.
When someone throws another task or patient your way, don’t just grin and bear it. Say this instead: “I’m at capacity right now. If it’s urgent, let’s prioritize it. If not, we’ll need to revisit it later.” You don’t need to apologize or over-explain. You’re not being difficult—you’re being realistic.
These boundaries aren’t just about making your workday easier. They’re about saving your energy for the things—and the people—that matter most.
4. Prioritize restorative sleep:
Enough sleep is one of the first things to go when life gets overwhelming, but here’s the reality: you can’t function—let alone thrive—without it. You’ve probably felt it. The foggy brain, the short temper, the physical exhaustion that no amount of coffee can fix. Sleep isn’t just rest; it’s your body’s way of resetting.
Aim for 7–9 hours a night, even if it means making changes. Set a bedtime routine that signals your body it’s time to wind down. Blackout curtains, calming rituals, and no screens before bed can work wonders. Protecting your sleep isn’t indulgent—it’s necessary to face the demands of your day with clarity and strength.
5. Fuel your body:
Put that coffee down! Grabbing quick snacks or living on caffeine might feel like the easiest option, but it’s not helping you in the long run. Food is fuel, and your body needs steady energy to keep up with the mental, emotional, and physical demands of your work.
Focus on whole, nutrient-dense foods that nourish you: lean proteins, whole grains, and plenty of fruits and vegetables. And drink water—more than you think you need. Staying hydrated and well-fed doesn’t just keep you going; it keeps you feeling steady and capable.
6. Incorporate movement:
No, we don't mean hitting the gym for hours or committing to a grueling routine. It’s about moving your body in a way that feels good and helps you let go of the tension you’re carrying.
Even a 10-minute walk outside can clear your mind and release stress. Try stretching after a long day, doing a quick yoga session in your living room, or simply dancing to your favorite song. Movement isn’t another obligation—it’s a gift to yourself, a moment to breathe and reconnect with your body.
7. Find your people
Burnout isolates you. It convinces you that you’re the only one struggling, but that couldn’t be further from the truth. You need people in your corner—people who understand, who listen, and who remind you that you don’t have to do this alone.
Seek out a support network, whether it’s a group of PMHNPs who know exactly what you’re going through or a trusted mentor who can guide you. Lean on your friends and family, too. Sometimes just having someone say, “I hear you,” can ease the weight you’re carrying.
8. Rediscover what lights you up
When you’re in the thick of burnout, everything starts to feel like a chore—even the work you once loved. But you didn’t choose this career by accident. Somewhere along the way, it meant something deeply personal to you.
Take a step back and think about those moments when you’ve made a difference—when a patient’s progress or a kind word reminded you why you do this. And don’t stop there. Make time for the parts of life that bring you joy outside of work. Whether it’s painting, hiking, cooking, or just spending time with loved ones, reconnect with the things that remind you you’re more than your job.
9. Get help when you need it
Let’s stop pretending you have to handle everything on your own. Carrying the emotional load of your work day in and day out is heavy—too heavy for anyone to bear without support. Burnout can coexist with mental health conditions such as depression, anxiety disorders, and PTSD.
If you’re feeling overwhelmed, reach out. Therapy can help you process the emotional weight of your job and develop tools to manage stress. The parental burnout inventory is an example of an assessment tool that can provide insights into managing burnout. If your workplace offers wellness programs, use them. This isn’t about admitting defeat; it’s about recognizing that even the strongest people need help sometimes.
Asking for support doesn’t make you less capable—it makes you human. And you deserve care, just as much as the patients you care for every day.
10. Take breaks ... real ones!
Do you feel like you’re running on autopilot, going from one task to the next without stopping to catch your breath? It’s easy to get stuck in that cycle, convincing yourself you don’t have time for a break. But here’s the thing: you can’t keep pouring from an empty cup.
Breaks are not optional; they’re essential. Taking even ten minutes to disconnect can lower stress, reset your focus, and give you the energy to power through the rest of your day. Go for a short walk, sit in silence, or just close your eyes and practice deep breathing. It doesn’t have to be elaborate—it just has to be intentional.
And let’s talk about vacations. If you’ve been putting off PTO because “things are too busy,” it’s time to reevaluate. Taking time off isn’t slacking; it’s ensuring you come back recharged and ready to give your best.
A burned-out PMHNP doesn’t help anyone—not your patients, not your team, and definitely not you. So, step away. The world will keep spinning while you rest.
Why preventing burnout matters?
As PMHNPs, job burnout is a complex issue characterized by professional exhaustion and a loss of interest in work—it’s a threat to everything that makes you effective at your job.
When you’re burned out, it’s harder to connect with patients, make sound clinical decisions, and stay present in the moment. Your patience wears thin, your empathy feels forced, and the job that once felt meaningful starts to feel like an uphill battle every single day.
And it doesn’t stop at work. Burnout follows you home. It eats into your personal life, leaving you too exhausted to spend time with your family, enjoy your hobbies, or even take care of yourself. It’s not just about feeling tired—it’s about feeling like you’re losing control of your life.
Burnout also has real consequences for your health. Left unchecked, it can lead to anxiety, depression, and even physical health problems like high blood pressure or chronic fatigue.
For PMHNPs, this isn’t just about you—it’s also about your patients. They rely on you to be focused, present, and capable. If burnout compromises that, everyone pays the price.
Preventing burnout isn’t optional. It’s about protecting your ability to care for others while also caring for yourself. You can’t give your best if you’re running on empty.
Finally, you don’t have to do this alone
Becoming a psychiatric nurse practitioner isn’t just a career—it’s a calling. But balancing coursework, work, and life while trying to secure a clinical placement can feel impossible. That’s why nphub.com exists: to make this part of your journey easier.
We connect PMHNP students with preceptors who understand the demands of mental health care. With our help, you can skip the endless searches and focus on gaining the experience you need to graduate and thrive in your career.
You’ve chosen to support others in their toughest moments. Let us support you in yours. Explore how we can help at nphub.com.
Looking to learn more about nursing? Be sure to explore our collection of guides and resources here.
Find a preceptor who cares with NPHub
Book a rotation.webp)








.webp)

.webp)



.webp)