Ever had a patient nod along as you explain their care plan, only to ask five minutes later, “Wait… so what am I supposed to do?” Yeah, we’ve all been there
Patient education is one of the most important (and most underrated) parts of nursing, yet it often gets rushed, overlooked, or drowned out by medical jargon.
It’s a reality that patients need both information and understanding and every day nurses deliver critical details about medications, treatments, and lifestyle changes, yet many patients leave feeling confused or overwhelmed.
Strong patient education empowers individuals to take control of their health, improving outcomes and reducing preventable complications. It also builds trust, making patients more likely to follow through with their care plans. To be truly effective educators, nurses must go beyond delivering instructions. They must engage, simplify, and tailor their approach to meet the unique needs of each patient through effective patient education.
So, how do you take your patient education skills from “Here’s a pamphlet” to “Let me make this easy for you”? Let’s talk about it.
Why are Nurses responsible for patient education?
Think about the last time a patient looked at you with that “I have no idea what you just said” expression. It happens all the time. Whether it’s a new diagnosis, a complicated medication schedule, or just trying to make sense of their symptoms, patients are often overwhelmed and unsure of what to do next.
This responsibility falls on nurses because health literacy is a major factor in patient outcomes. Studies show that patients with low health literacy struggle to make informed decisions, manage chronic conditions, and follow prescribed treatments. When patients don’t fully understand their health, the risks increase - missed medications, improper wound care, unmanaged diseases, and preventable hospital readmissions. And while online health information is abundant, much of it is misleading, outdated, or overly complicated, making it even harder for patients to separate facts from fiction.
Nurses play a critical role in bridging this gap. They spend more time with patients than most other healthcare providers and are uniquely positioned to break down complex medical information in a way that makes sense.
Unlike rushed physician visits or dense discharge instructions, nurses can assess patient comprehension in real time and adjust their explanations to fit the individual’s needs. Tailored education is key because factors like age, language, culture, and education level all impact how well a patient absorbs information. Simple language, visual aids, and communication techniques like the teach-back method ensure that patients not only hear the information but actually understand and retain it.
Also, patient education builds confidence and promotes self-efficacy. Patients who feel informed are more likely to engage in their own care, adhere to treatment plans, and make proactive health decisions. Nurses don’t just instruct; they empower.
At a time when the healthcare system is stretched thin and patient loads are higher than ever, effective education it’s key. Well-informed patients require fewer emergency visits, experience better long-term health outcomes, and ultimately make the entire healthcare process more efficient for everyone involved.
That’s why nurses aren’t just caregivers; they’re educators, advocates, and the key to improving patient health literacy.
How can NPs (and other types of nurses) become better educators?
Both NPs and RNs guide patients through the maze of medical information, breaking it down in a way that actually makes sense. But being a great patient educator goes beyond handing someone a pamphlet and hoping for the best, its important to make sure that patients ACTUALLY get it.
Yes, you can explain something ten times, but if a patient walks out and still thinks their antibiotics are for a viral infection, we’ve got a problem.
Some patients come in eager to learn, while others are overwhelmed, scared, or convinced that the internet knows more than you do (thanks, Google). And in a world where misinformation spreads faster than a bad case of the flu, nurses have never been more essential in guiding patients toward the right health decisions.
Effective patient education is crucial for enhancing patient care, ensuring that patients and their families are well-informed and engaged in the healing process.
So, how do you make sure your teaching sticks? Here’s how to refine your approach and make patient education a powerful, effective part of your nursing practice.
1. Assess each patient’s health literacy level (don’t assume they understand)
Not all patients process health information the same way and some will fake understanding just to avoid feeling embarrassed.
To educate patients effectively, nurses need to first gauge a patient’s level of health literacy or their ability to understand, evaluate, and use health information so instead of assuming they get it, meet them where they are:
- Ask what they already know about their condition or treatment. No sense explaining insulin injections for ten minutes if they don’t even understand what diabetes is.
- Watch their response. Do they look engaged or lost? Are they asking questions or just smiling and nodding?
- Check for barriers. Some patients struggle with low literacy, hearing impairments, language differences, or plain old anxiety—any of which can make education harder.
If a patient doesn’t fully understand their health, they won’t be able to manage it. So before diving into explanations, figure out what they actually need from you.
2. Speak clearly and ditch the jargon
Medical professionals speak a whole different language, and half the time we don’t even notice. But if you’re tossing around terms like hypertension, myocardial infarction, or polypharmacy, don’t be surprised when your patient zones out.
Nurses should focus on using plain, simple language and avoiding complex terminology whenever possible. Teaching patients effectively requires clear communication. Some key techniques to keep it clear include:
- Lose the fancy words. Say high blood pressure instead of hypertension, swelling instead of edema, and heart attack instead of myocardial infarction.
- Use the teach-back method. Instead of asking, Do you understand? (because they’ll say “yes” even if they don’t), say, Can you explain it back to me in your own words?
- Slow it down. You might have a tight schedule, but if a patient leaves confused, they’ll either come back with complications or call with more questions—so taking time upfront actually saves you time.
- Pay attention to body language. If they look lost, they probably are.
A good rule? If you wouldn’t explain it that way to a friend or family member, it’s too complicated. Good communication ensures patients aren’t just nodding along but truly grasping their health information.
3. Make information accessible and culturally relevant
Health literacy it’s shaped by cultural, social, and economic factors and nurses should adapt their educational approach to meet patients where they are. Health care providers must ensure that information is accessible and culturally relevant to all patients. Not everyone learns the same way, some need visuals, others need hands-on practice, and some just need you to break it down real simple.
And beyond learning styles, cultural beliefs and personal experiences shape how patients receive health information so to make education more effective:
- Use visual aids like diagrams, videos, and models can make things click better than words alone.
- Offer materials in their language. If they don’t fully understand English, a well-translated document (or a medical interpreter) can make all the difference.
- Respect cultural beliefs. Some patients may have concerns about medications, treatments, or procedures that go against their religious or cultural beliefs. Address these with sensitivity instead of shutting them down.
- Ask open-ended questions. Instead of, Do you understand?, try What will you do when you get home? That way, you really know if they got the message.
When patients feel like you’re speaking to them not at them they’re more likely to absorb and apply what you’re teaching and are more likely to be engaged and receptive to learning.
4. Recognize the real-world barriers patients face
Here’s the thing: Even when patients do understand their health, that doesn’t mean they can always act on it. Money, transportation, family responsibilities, and mental health struggles can all get in the way.
Instead of just giving instructions, help problem-solve:
- Ask about financial struggles. A patient might not be skipping meds because they don’t care, they might just not be able to afford them. If cost is a barrier, connect them with resources.
- Consider accessibility. If a patient can’t drive to follow-ups, they may need telehealth options or local resources for transportation.
- Recognize motivation levels. If a patient is feeling helpless, overwhelmed, or just burnt out, they may need extra support and encouragement, not just more instructions.
- Know that life gets in the way. You can give the best education in the world, but if a single mom has to choose between picking up her meds or feeding her kids, we know which one comes first. Empathy goes a long way.
Education works best when it fits into a patient’s real life, not just an idealized version of what we think they should be doing. By recognizing and addressing these influences, nurses can customize education to fit the patient’s real-life circumstances which increases the likelihood that they’ll follow through with care plans. Nursing management plays a critical role in recognizing and addressing these barriers to successful patient education.
5. Make effective patient education a core skill
Being a great educator it’s a fundamental part of nursing and even thought nursing school teaches how to take vitals, assess symptoms, and administer treatments many nurses receive little formal training in health literacy and patient education. The essential role that nurse educators play in promoting health literacy cannot be overstated, as they are crucial in preparing future nurses and engaging patients in meaningful education.
This creates a challenge: if patients don’t understand their care, even the best treatment won’t help them. So how do we fix that?
- Advocate for stronger training in nursing programs. New nurses should graduate with a solid foundation in patient education strategies—not just clinical skills.
- Seek out continuing education on communication and teaching techniques. Workshops, courses, and certifications in health literacy can refine your ability to educate effectively.
- Integrate education into daily nursing practice. Teaching shouldn’t just happen during discharge, it should be a continuous part of every interaction with patients.
- Collaborate with colleagues. Sharing best practices with fellow nurses can help create a stronger culture of patient-centered education within healthcare teams.
The more health literacy is prioritized in nursing education and practice, the better outcomes patients will experience.
Is it bad to let patients do their own research?
Patients today don’t just rely on healthcare providers for answers, they turn to the internet first. Some come in with solid questions based on reliable sources, while others arrive convinced they have a rare condition after falling into a rabbit hole of misinformation.
So, should nurses be concerned about patients doing their own research? Not necessarily. The issue isn’t that patients are looking for information—it’s where they’re getting it from.
Instead of discouraging research, nurses should guide patients toward accurate, trustworthy sources and help them make sense of what they find. Nurse leaders play a pivotal role in this process by ensuring that patient education is prioritized and that patients are directed towards reliable information, even amidst challenges like staffing shortages and demanding workloads.
Don’t dismiss, redirect them.
When a patient confidently states, “I read online that my symptoms mean I have [insert worst-case scenario],” it’s tempting to shut it down. But brushing off their concerns won’t make them trust you more, it may actually push them further into misinformation.
Instead, turn their research into a productive conversation:
- Acknowledge their effort. Patients who look up their symptoms are taking an active role in their health, which is something nurses should encourage. Instead of saying, “That’s not accurate,” try, “I love that you’re looking into this. Let’s go over what you found together.”
- Ask where they got their information. A reputable medical website? A Facebook post? Understanding the source helps determine how much guidance they need. Nurses play a crucial role as facilitators in helping patients access, understand, and evaluate health information.
- Guide them toward credible sources. Promoting patient education by guiding them to reliable sources is essential. Many patients don’t realize how much misinformation is out there. Directing them to trusted sites like the CDC, Mayo Clinic, NIH, or disease-specific organizations ensures they have reliable information. Providing accessible and understandable health information empowers patients to make informed decisions.
Help patients evaluate online information
Not all health information online is bad, but many patients don’t know how to separate fact from fiction to improve patient outcomes.
Some sites are backed by science, while others push fear-based narratives or sell unproven treatments. Nurses must help patients critically evaluate what they read, and encourage them to ask these questions before trusting an online source:
- Who wrote it? Is the information from a licensed medical professional or someone with no credentials? Nurses can improve patients’ health literacy by teaching them how to assess credible sources.
- Is it backed by science? Does the site cite actual research and medical studies, or just personal anecdotes? Evaluating health information is essential for empowering patients to make informed decisions.
- Is it selling something? If an article promotes a “miracle cure” that only they can provide, it’s probably more marketing than medicine. Patients need guidance on identifying bias in online health content.
- Does it align with reputable sources? If trusted organizations like the CDC or WHO don’t mention it, be skeptical. Nurses should advocate for health literacy to help patients navigate conflicting health information.
Misinformation spreads quickly, but giving patients the tools to assess credibility can help them make better health decisions.
Address fear and misinformation with facts
Patients don’t always research health topics out of curiosity; sometimes, they’re scared. Whether it’s a newly diagnosed condition, a medication they don’t trust, or a viral health myth, fear can make patients vulnerable to misinformation, which can compromise patient safety.
When patients bring up misleading or inaccurate health claims, the best approach is:
- Empathy. Instead of dismissing their concerns, validate them. “I can see why that would be concerning. Let’s go over what we actually know from medical studies.” Nurses must recognize that sociodemographic and motivational factors influence health literacy, including fear and misinformation.
- Clarity. Break down the misinformation and provide science-backed explanations that are easy to understand. Using plain language and visual aids can help patients better grasp the facts.
- A trusted alternative. Instead of just saying, “That’s wrong,” offer a reliable resource where they can find accurate information. Nurses should reinforce correct health information through ongoing patient education, not just one-time conversations.
Encourage patients to take an active role in their health
Patients who research their health want the right answers so instead of shutting down their curiosity, nurses and nurse educators can encourage patients to take an active role by:
- Giving them recommended reading. If they’re interested in learning more, point them toward trustworthy sites or patient education materials. Helping patients find accessible information empowers them to take control of their health.
- Teaching them how to ask the right questions. Encouraging patients to ask about risks, benefits, and evidence behind treatments helps them feel more confident in their care.
- Reinforcing their role in decision-making. Patients who feel informed are more likely to follow through with treatment plans and engage in their own health management. Nurses must equip patients with self-efficacy strategies so they feel in control of their health decisions.
The internet isn’t going anywhere, and neither is patient research. Nurses should see it as an opportunity to educate, guide, and build trust. By helping patients identify credible sources, evaluate information, and ask the right questions, nurses support health literacy and empower patients to make better healthcare decisions.
What should nurses avoid when educating patients?
Avoid using fear as a motivational tool
It’s tempting to emphasize worst-case scenarios to push patients into action, but using fear as a tactic often leads to anxiety, denial, or avoidance rather than real understanding. Patients who feel overwhelmed by negative messaging may disengage from care entirely, looking for alternative solutions that feel less intimidating—even if they’re not medically sound.
A better approach is to focus on empowerment. Patients need to understand the consequences of their choices, but they also need to feel like they have control over their health. Rather than saying, “If you don’t take your medication, you’ll end up in the hospital,” a more effective approach would be, “Taking your medication consistently will help you avoid complications and keep you feeling your best.” When education is framed in a way that encourages action without inducing fear, patients are more likely to absorb and apply what they’ve learned.
Don´t overload patients with too much information at once
Patients are often given a flood of medical information during a single visit, especially after a new diagnosis. While nurses may feel obligated to explain everything at once, too much information can overwhelm patients, making it harder for them to retain even the most important details. This cognitive overload can cause frustration, leading some patients to tune out or misunderstand key aspects of their care.
Instead, prioritization and simplification are key. The most critical takeaways should be identified so patients can focus on what is immediately necessary, with additional information introduced gradually. Education should be spaced out over multiple interactions rather than crammed into a single session. Using plain language, analogies, or visuals to reinforce key points makes it easier for patients to retain and recall information when they need it. Breaking instructions into manageable steps ensures that patients can actually implement what they’ve learned rather than feeling lost in a sea of details.
Dont relying only on verbal instructions
Many nurses rely primarily on spoken explanations when educating patients, assuming that speaking clearly is enough. However, verbal instructions alone are easy to forget, especially when a patient is stressed, anxious, or processing new information. Studies show that people retain only a fraction of what they hear, meaning much of what is said during an appointment might not stick. This is particularly problematic for patients managing chronic conditions or complex treatment regimens.
Reinforcing education through multiple formats significantly improves comprehension and adherence. Providing written instructions in simple, easy-to-follow language allows patients to review information at their own pace. Visual aids like diagrams, models, or demonstration videos can clarify complex medical concepts. Encouraging patients to take notes or have a family member present during discussions provides an extra layer of reinforcement. When patients receive structured materials they can reference later, they are far more likely to follow through with their care instructions, leading to better long-term health outcomes.
Make sure patients feel comfortable asking questions
Many patients hesitate to ask for clarification, either because they don’t want to seem difficult, feel rushed, or simply don’t know what they don’t know. If a patient doesn’t fully understand their diagnosis or treatment plan but is too intimidated to ask for more details, they may leave the visit with major gaps in understanding. This can result in non-compliance with treatment, preventable complications, and unnecessary follow-up visits.
Creating a safe space for patients to ask questions is crucial for effective education. Instead of simply asking, “Do you have any questions?”—which many patients may say no to out of politeness or embarrassment—nurses should say, “I know this is a lot of information. What can I explain more clearly?” This small change encourages patients to engage without feeling self-conscious. Normalizing curiosity by saying, “A lot of my patients ask about this—would you like to go over it in more detail?” helps remove the stigma of not understanding. Offering follow-up opportunities, such as providing contact information for further questions or suggesting a second appointment to reinforce education, ensures that patients feel supported beyond the initial conversation.
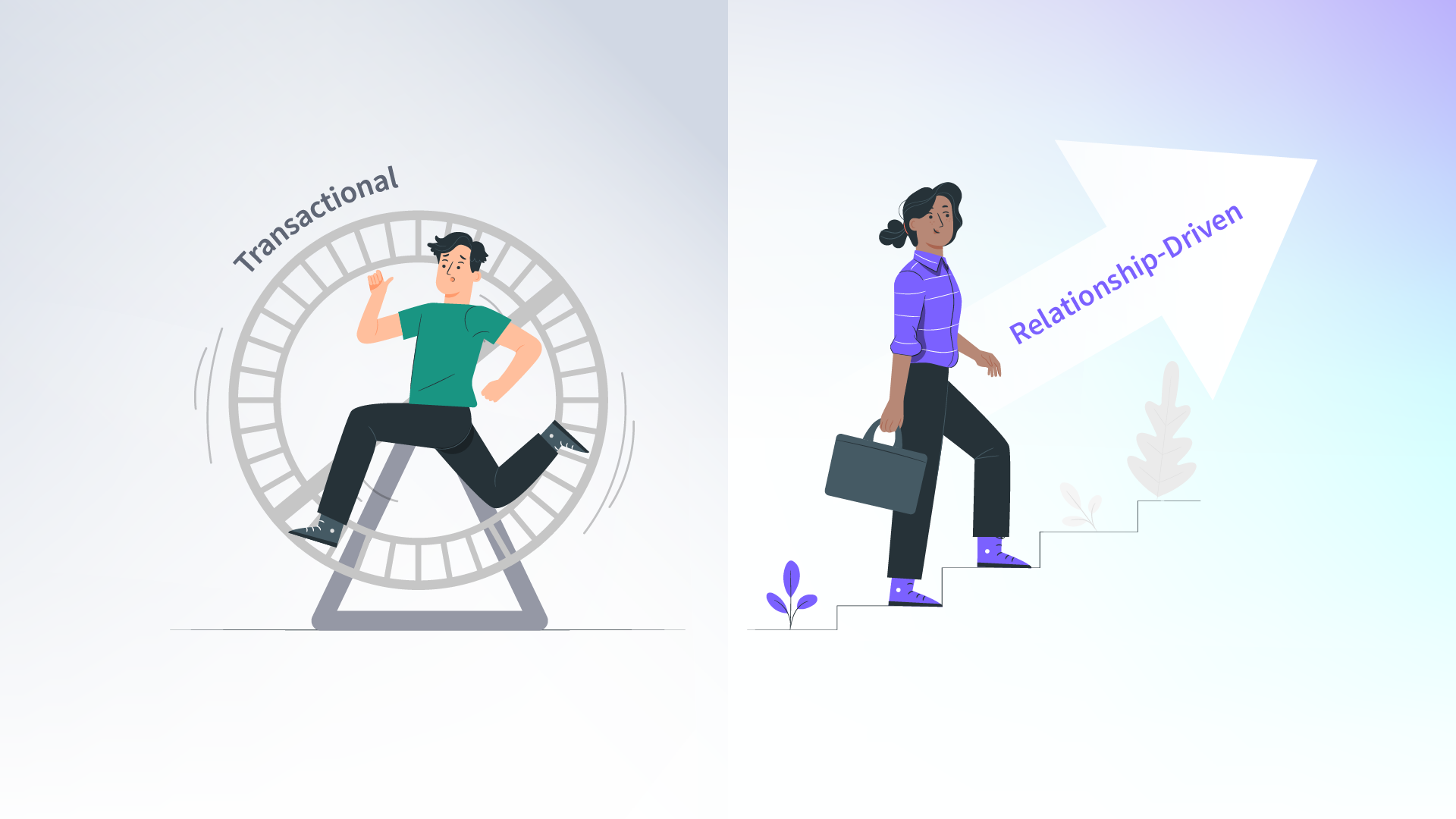
Avoid treating patient education as a one-time event
One of the biggest mistakes in patient education is treating it as a single conversation rather than an ongoing process. Health information is complex, and expecting patients to grasp everything in one sitting is unrealistic. Some conditions require continuous education as the patient’s needs evolve, and reinforcement is necessary to prevent misunderstandings and ensure adherence to treatment.
Education should be an integral part of every interaction with the patient. Key points should be reinforced during multiple visits rather than assuming patients remember everything from their first consultation. Regular check-ins and follow-up questions should be used to assess retention and adjust explanations as needed. Additionally, adapting education to match the patient’s preferred learning style—whether through hands-on demonstrations, written materials, or digital resources—improves understanding. When patient education is treated as a long-term conversation rather than a one-time lecture, patients feel more supported, confident, and prepared to take control of their health.
What else can I do to become a better patient educator?
Nurses today have more tools than ever to enhance their role as patient educators. Beyond traditional face-to-face interactions, there are countless ways to improve how you teach, share information, and make a lasting impact on your patients and even fellow healthcare professionals.
Whether it’s through refining your communication skills, using technology, or expanding your reach beyond the bedside, here are some strategies to take patient education to the next level.
One of the most effective ways to improve as an educator is to refine your communication techniques. Studies show that using clear, jargon-free language, engaging patients in open discussions, and confirming understanding through methods like teach-back significantly improves health literacy and patient outcomes.
Instead of assuming patients understand, ask them to explain information in their own words and watch for verbal and non-verbal cues that may indicate confusion. The more comfortable and confident patients feel in asking questions, the better they’ll retain what you teach them.
Another way to strengthen your skills is to tailor education to each patient’s needs. Every patient has a unique learning style, and factors such as age, education level, language proficiency, and cultural background play a role in how they absorb information.
Using visual aids, written materials, hands-on demonstrations, and digital resources can make learning more accessible, especially for patients with limited health literacy. Additionally, recognizing and addressing social determinants of health, like financial barriers or lack of access to resources, helps ensure that patients are not just informed, but also equipped to act on that information.
If you’re passionate about education, consider expanding your impact beyond individual patient interactions. Many nurses today are using social media, blogs, and video platforms to share reliable health information with a wider audience.
You might consider creating educational content on platforms like YouTube, Instagram, or TikTok, where healthcare professionals are building communities and helping to combat misinformation. Patients often turn to online sources for medical advice, so having more trusted professionals providing accurate, engaging, and accessible health education can make a significant difference.
For those who enjoy teaching, there are also formal opportunities to step into an educator role. Becoming a Nurse Educator allows you to guide the next generation of nurses, helping them transition from academic settings into clinical practice.
Whether you teach in a nursing school, lead workshops, or mentor new nurses in a hospital setting, the ability to shape future healthcare providers can be just as fulfilling as educating patients.
Additionally, continuing education and professional development can strengthen your teaching abilities. Taking online courses in communication, patient education, and health literacy can help refine your skills. Many nursing organizations offer training on cultural competence, digital health literacy, and strategies for engaging different patient populations. The more knowledge you gain, the better equipped you’ll be to explain complex medical concepts in a way that makes sense to patients.
Patient education is more than just a duty—it’s an essential part of improving healthcare outcomes. Whether you focus on refining your bedside teaching skills, creating online educational content, stepping into a formal educator role, or continuing your own education, investing in your ability to educate makes a lasting impact.
At the core of nursing is the ability to empower, inform, and guide patients toward better health, and the more skilled you become at teaching, the more lives you can change.
Follow NPHub on social media:
Facebook: https://www.facebook.com/NPHubOfficial/
Instagram: https://www.instagram.com/nphub_
Find a preceptor who cares with NPHub
Book a rotation.webp)







.webp)

.webp)



%20(3)%20(2).svg)
.webp)