The healthcare landscape continues to evolve, and one of the most common questions patients and aspiring medical professionals ask is about the differences between nurse practitioners (NPs) and medical doctors (MDs). While both healthcare providers play crucial roles in disease prevention and patient care, their educational backgrounds, clinical experience, and practice authority create distinct professional paths.
Key Similarities:
- Both can treat patients and provide direct patient care
- Ability to prescribe medications and interpret diagnostic tests
- Focus on health promotion and disease prevention
- Can serve as primary care providers
- Board certification requirements
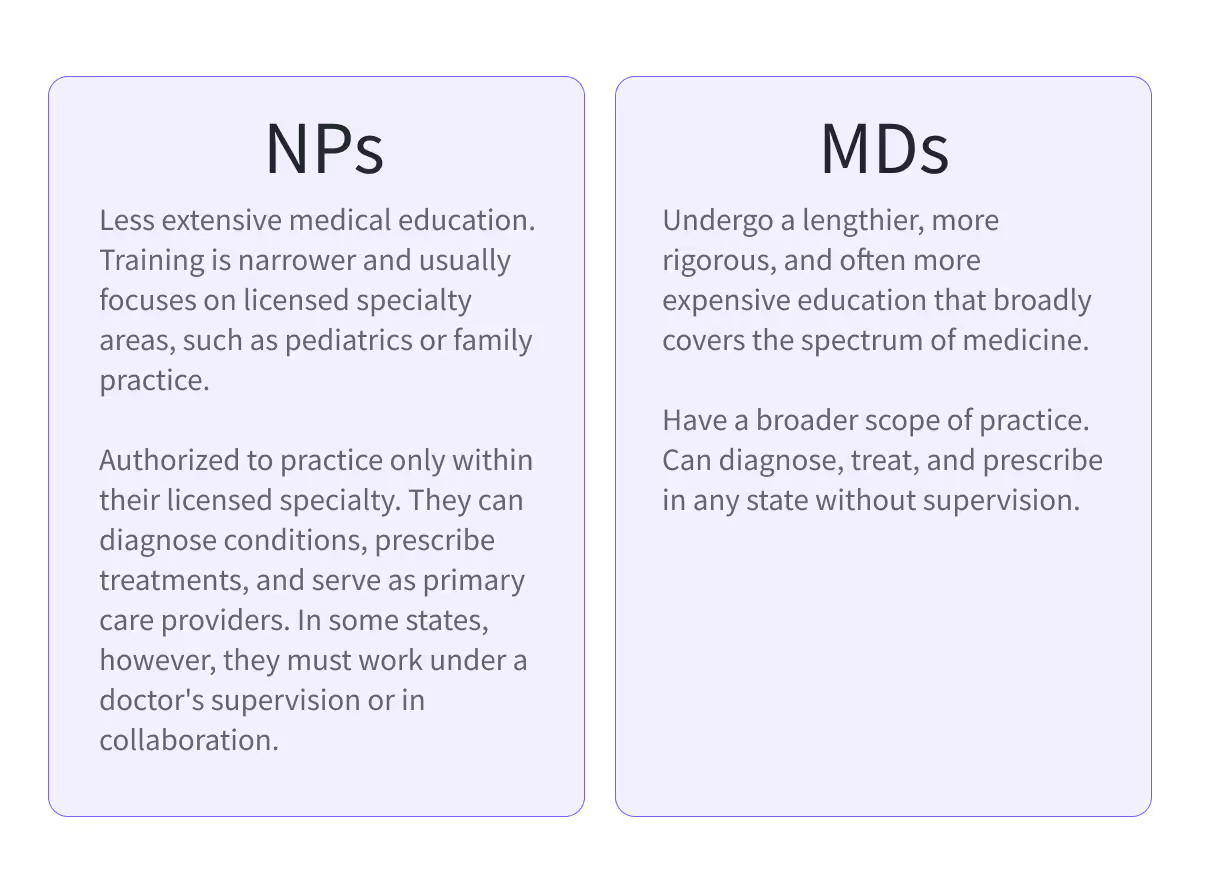
Key Differences:
- Educational pathway length and requirements
- Clinical rotation hours and experience
- Practice authority varies by state for NPs
- Approach to patient care (nursing model vs medical model)
- Specialty training requirements
As primary care providers, both NPs and MDs can prescribe medications, interpret diagnostic tests, and manage treatment plans. However, their approaches often differ: NPs typically follow a nursing model that emphasizes health promotion and preventive care, while MDs pursue extensive training in disease diagnosis and medical specialty areas.
This article examines the fundamental differences between these two career paths, from educational requirements and clinical rotations to scope of practice and practice authority. Whether you're considering a career in healthcare or seeking to better understand your care options, we'll unravel the unique value each provider brings to patient care.
Career Differences: A Deeper Understanding of NP vs MD Roles
Understanding the career distinctions between nurse practitioners and medical doctors helps clarify their unique contributions to healthcare delivery. While both healthcare providers are essential to our medical system, their approaches and practice parameters differ significantly.
Core Practice Differences
NPs typically follow a patient-centered nursing model emphasizing health promotion and disease prevention, while MDs focus on a medical model of disease diagnosis and treatment. Both NPs and MDs operate in primary and specialty care settings, providing comprehensive healthcare services across various medical fields. Both healthcare providers can interpret diagnostic tests and manage treatment plans, but their philosophical approaches often differ.
Key distinctions include:
- MDs primarily focus on disease diagnosis, treatment, and specialty procedures
- NPs emphasize holistic patient care, prevention, and health education
- Both manage acute and chronic conditions effectively
- NPs often dedicate more time to patient education and lifestyle counseling
- MDs typically handle complex medical cases and specialized treatments
Clinical Authority
MDs maintain consistent practice authority across all states, while NPs' ability to practice independently varies by location. In 27 states, nurse practitioners can practice independently, managing patient care and prescribing medications without physician supervision. Other states require varying levels of physician oversight for NP practice.
Practice environments include:
- MDs: Private practices, hospitals, academic medical centers
- NPs: Primary care offices, community clinics, healthcare systems
- Both: Emergency departments, outpatient facilities, specialty clinics
- Different oversight requirements for prescribing medications
Patient Care Approach
Both providers deliver comprehensive patient care through different methodological approaches. While MDs emphasize diagnostic precision and specialized treatment protocols, NPs often focus on the whole-person approach to healthcare delivery.
Common responsibilities include:
- Conducting thorough physical examinations
- Taking comprehensive medical histories
- Ordering and interpreting diagnostic and lab tests
- Creating and managing treatment plans
- Providing health education and preventive care
- Prescribing medications and monitoring outcomes
- Coordinating care with other healthcare providers
This framework sets the foundation for understanding the more specific differences in education, clinical training, and practice authority that we'll explore in subsequent sections.
Roles and Responsibilities in Modern Healthcare
Primary Care Settings
Nurse practitioners serve as primary care providers, managing a wide range of patient needs. Their scope includes performing health assessments, developing treatment plans, and coordinating patient care. They offer comprehensive services from routine check-ups to managing chronic conditions.
Primary care medical doctors deliver similar services but with broader diagnostic authority and the ability to handle more complex medical cases independently. Their consistent state-to-state authority enables seamless practice across jurisdictions.
Supervision and Leadership
While both providers manage treatment plans and prescribe medications, their supervisory roles differ. MDs often lead medical teams and oversee other healthcare providers, including nurse practitioners in certain states. NPs frequently supervise registered nurses and support staff, particularly in primary care settings.
Full Practice Authority: Understanding State-by-State Regulations
The scope of practice authority for Nurse Practitioners (NPs) has evolved dramatically in recent years, significantly impacting how NPs deliver patient care across the United States. As of 2025, states now fall into three distinct categories that determine how independently NPs can practice.
Full Practice States
In 34 states and the District of Columbia, NPs enjoy Full Practice Authority (FPA), meaning they can:
- Evaluate and diagnose patients independently
- Order and interpret diagnostic tests
- Initiate and manage treatments
- Prescribe medications without physician oversight
- Practice under the exclusive authority of the state board of nursing
This shift toward greater autonomy reflects national efforts to address healthcare provider shortages, particularly in rural and underserved areas, and to improve patient access to high-quality care.
States newly adopting Full Practice Authority since 2020 include: Massachusetts, Pennsylvania, Kansas, Ohio, Texas, Indiana, Tennessee, Michigan, Alabama, Louisiana, South Carolina, and Wisconsin.
Reduced Practice States
In 12 states, NPs operate under Reduced Practice Authority. These states require:
- Career-long or condition-specific collaborative agreements with physicians
- Physician oversight for certain elements of clinical practice
- Limited prescriptive authority in specific circumstances
- Restrictions on independent practice settings
Although NPs in these states have some autonomy, their ability to provide immediate and complete patient care is still constrained by formal collaboration requirements.
Restricted Practice States
In 4 states, the most stringent regulations apply, requiring:
- Mandatory physician supervision for all patient care activities
- Delegation of authority by supervising physicians
- Team-based management of treatment plans
- Restricted ability to prescribe medications independently
NPs in restricted practice states face significant limitations, which can delay access to medical services, particularly for patients in rural or underserved communities where physician shortages are most acute.
Why Full Practice Authority Matters
The move toward Full Practice Authority has already demonstrated measurable benefits:
- Improved Access to Care: Rural areas in FPA states have seen a 45% greater increase in NP practice locations compared to restricted states.
- Reduced Costs: Healthcare systems in FPA states report an average 11% reduction in primary care costs.
- Shorter Wait Times: Wait times for primary care appointments decreased by an average of 8 days within two years of FPA adoption.
- Better Chronic Disease Management: Hospitalization rates for manageable chronic conditions like heart disease and diabetes decreased by 7–12% where NP-led care expanded.
In short, expanding NP authority isn't just a win for providers it's a win for patients, public health, and the future of accessible healthcare in America.
Healthcare Practice Settings and Environments
Both NPs and MDs serve patients across diverse healthcare settings, each bringing their expertise to different environments.
Primary Care Settings
Nurse Practitioners:
- Group medical practices focusing on family health
- Community health centers
- Retail clinics providing accessible care
- School-based health centers
- Rural health clinics
Medical Doctors:
- Private solo practices
- Group medical practices
- Academic medical centers
- Primary care clinics
- Rural health facilities
Specialty and Hospital Settings
Both providers work in:
- Inpatient hospital departments
- Outpatient specialty clinics
- Emergency departments
- Urgent care centers
- Surgical centers
Unique Practice Environments
NPs often serve in:
- Public health departments
- Corporate wellness centers
- Home health services
- Long-term care facilities
MDs frequently practice in:
- Research institutions
- Teaching hospitals
- Specialty surgical centers
- Military medical facilities
Licensure and Specialization
Healthcare providers follow distinct paths to obtain their licenses. MDs complete four years of medical school, followed by residency training before obtaining a medical license. They can choose between an MD degree or a DO degree, with DOs receiving additional training in osteopathic medicine and the musculoskeletal system.
NPs start as registered nurses and then pursue advanced degrees—either a Master of Science in Nursing (MSN) or a Doctor of Nursing Practice (DNP). Upon graduation, they must obtain board certification and state licensure to practice.
Specialization Options
Advanced Practice Nursing Specialties:
- Family Nurse Practitioner (FNP)
- Adult-Gerontology Primary Care
- Pediatric Primary Care
- Women's Health
- Psychiatric Mental Health
- Acute Care
- Emergency Care
Medical Doctor Specialties:
- Internal Medicine
- Family Medicine
- Surgery
- Pediatrics
- Obstetrics/Gynecology
- Emergency Medicine
- Psychiatry
Board Certification Process
Both providers must maintain their credentials through continuing education and regular recertification. NPs obtain national board certification through specialized nursing boards, while MDs receive certification through medical specialty boards. Both must demonstrate ongoing competency in their respective fields to maintain their practice privileges.
This comprehensive system of licensure and specialization ensures that both NPs and MDs are qualified to provide safe, effective care within their scope of practice.
Education Timeline
Becoming a doctor can take 11-15 years, involving undergraduate programs, medical school, and three to seven years of residency.
For NPs, the journey starts with a 4-year undergraduate program to become Registered Nurses (RNs). After becoming RNs, they pursue a Master of Science in Nursing (MSN), which typically takes another 2-3 years.
Altogether, the NP education pathway amounts to around 6-7 years.
Education Costs and Debt
The financial commitment to become a healthcare provider varies significantly between NPs and MDs, reflecting their different educational pathways.
Medical Doctor Investment Cost Breakdown:
- Public medical schools: Average debt of $194,280
- Private medical schools: Average debt of $218,746
- Additional costs: Living expenses, study materials, licensing exams
- Residency application and interview expenses
- Board certification fees
- Educational Expenses:
- MSN programs: Average debt of $49,047
- Prior BSN debt: Approximately $28,917
- Certification exam fees
- Continuing education requirements
- State licensing costs
Salary Expectations

The income trajectory of nurse practitioners and medical doctors reflects their distinct educational paths and practice authority.
Nurse Practitioners are seeing strong earning potential as demand for primary and specialty care continues to rise. As of 2025, the average NP salary is approximately $153,285 per year, or about $12,773 per month. Top earners in the field can make upwards of $242,000 annually, reflecting the growing need for advanced practice providers across various healthcare settings.
Medical doctors continue to command high salaries, reflecting their extensive education and specialized training. As of 2025, the estimated total pay for a Medical Doctor is approximately $282,090 per year, with an average base salary of around $203,395 annually. The total earnings typically range between $213,000 and $379,000 per year.
Career progression varies by specialty choice and practice setting. NPs specializing in psychiatric mental health, acute care, or emergency medicine often command higher salaries. Similarly, MDs in surgical specialties, cardiology, and anesthesiology tend to earn more than those in primary care.
Geographic location significantly impacts earning potential for both providers. Urban areas and regions with healthcare provider shortages typically offer more competitive compensation. Additionally, both NPs and MDs can increase their earnings through leadership roles, performance bonuses, and specialized certifications.
Clinical Hours
NPs usually require 500-600 clinical hours, while medical school demands 6,000. Depending on the specialization, a 9,000-12,000-hour residency follows.
Nurse Practitioners and Medical Doctors are invaluable to the healthcare system, bringing unique skills, training, and perspectives to patient care.
By appreciating these differences, aspiring NPs can effectively navigate their journey in the medical field, leveraging the unique value that NPs bring to patient care.
If you're an NP student eager to further your journey, NPHub is here to assist. Securing your rotation hours is a significant step, and with NPHub, you can seamlessly book your preceptor
Join our community today and take a confident step toward your future as an NP.
Find a preceptor who cares with NPHub
Book a rotation.webp)







.webp)

.webp)



.webp)