TL;DR: The Big Question — Will Nurse Practitioners Replace Physicians?
- NPs are rising in primary care due to a severe physician shortage, especially in rural and underserved areas.
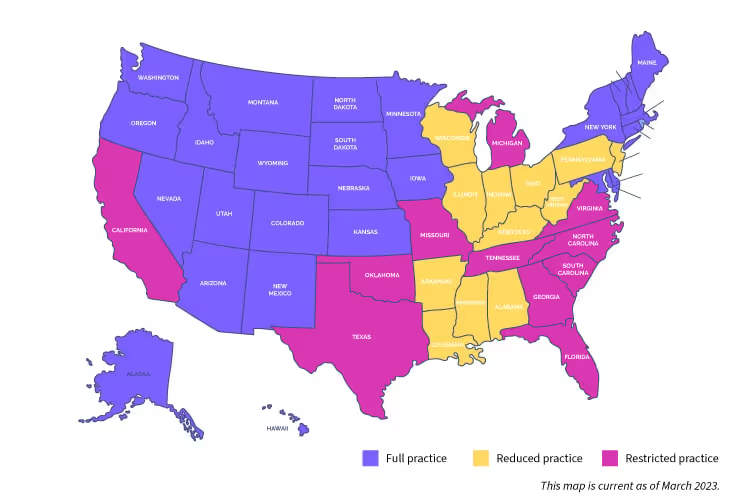
- Full Practice Authority (FPA) allows NPs to independently diagnose, treat, and prescribe in 34+ states.
- Studies show NP-led care is cost-effective, safe, and often equal in quality to physician care for routine and chronic conditions.
- NPs don’t “replace” physicians—they expand access and help relieve overloaded systems.
- The best model is teamwork: NPs handle day-to-day care, physicians focus on complex cases, and patients win.
As the healthcare industry rapidly evolves to meet growing patient needs, Nurse Practitioners (NPs) are stepping into increasingly significant roles. This shift has sparked a crucial dialogue: are nurse practitioners replacing doctors in the provision of primary care?
The rising prominence of NPs in healthcare is not a simple case of substitution, but rather a complex transformation of the healthcare landscape. This change is driven by several factors, including a looming physician shortage, the need for cost-effective care, and the push for improved patient access to medical services. Physicians undergo extensive medical training, including years of schooling and residency, which differ significantly from the training that nurse practitioners receive.
According to the Association of American Medical Colleges, the United States faces a projected shortage of 46,000 physicians. This shortage, particularly acute in primary care, has opened the door for nurse practitioners to fill critical gaps in patient care.
However, the question of whether NPs can or should replace physicians is nuanced and multifaceted. It requires a careful examination of the roles, capabilities, and limitations of both NPs and doctors within the broader context of our evolving healthcare system.
This article will explore the growing role of nurse practitioners in healthcare, focusing on the concept of Full Practice Authority (FPA) for NPs. We’ll weigh the benefits and potential drawbacks of expanding NP responsibilities, considering factors such as patient outcomes, cost-effectiveness, and the impact on overall healthcare delivery.
We aim to provide a comprehensive understanding of why nurse practitioners are increasingly seen as a solution to some of healthcare’s most pressing challenges while also acknowledging the irreplaceable role that physicians continue to play in complex medical care.
Addressing the Physician Shortage: NPs as a Cost-Effective Solution

The looming physician shortage presents a serious risk to the U.S. healthcare system, especially in primary care. The American Medical Colleges estimate that over the next decade, we could face a shortage exceeding 46,000 primary care physicians. This gap is particularly concerning in rural and underserved communities. As a result, nurse practitioners (NPs) and physician assistants (PAs) are stepping up in a significant role—helping to maintain access to quality patient care where it might otherwise falter.
A 2024 study found that nonphysician practitioners now account for roughly one-third of the nation’s active clinical workforce. Even more striking: the number of nurse practitioners and physician associates serving in Health Professional Shortage Areas grew from 72,000 in 2011 to 110,000 in 2023, while the number of practicing physicians in those areas stayed flat. This growth highlights how NPs and PAs are becoming indispensable in modern health care delivery—especially where primary care responsibilities are urgent, but physician-led care isn’t always available.
Rather than replacing physicians, NPs are working alongside them—offering cost-effective, timely access to care while still respecting clinical boundaries and collaborative roles, including:
- Diagnosing and treating common ailments
- Conducting and interpreting diagnostic tests
- Prescribing medications and developing treatment plans
- Managing chronic conditions
- Providing preventive care and patient education
In regions grappling with physician scarcities, particularly rural areas and underserved urban communities, nurse practitioners can ensure that essential healthcare remains accessible. Their ability to provide high-quality, patient-centered care at a lower cost makes them invaluable in addressing healthcare disparities.
In addition, studies have shown that NPs can provide many primary care services at a fraction of the cost of physician-led care without compromising on quality. This efficiency is crucial in an era of rising healthcare costs and strained budgets.
However, it’s important to recognize that while NPs can manage a wide range of primary care responsibilities, there are instances that require the specialized expertise of physicians. The goal is not for nurse practitioners to replace physicians entirely but to complement and extend the reach of the healthcare team.
By leveraging the skills of both NPs and physicians, the healthcare industry can create a more robust, accessible, and cost-effective system. This collaborative approach ensures patients receive appropriate care at the right level, optimizing outcomes and resources.
The Importance of Professional Boundaries in NP Practice
While nurse practitioners are increasingly filling gaps in primary care, a key aspect of their success lies in understanding and respecting the limits of their practice. This self-awareness is a hallmark of both NPs and physicians, contributing to patient care's overall quality and safety.
For nurse practitioners, recognizing these boundaries means:
- Acknowledging when a patient's condition exceeds their scope of practice
- Making timely referrals to specialists or primary care physicians when necessary
- Collaborating effectively with other healthcare professionals to ensure comprehensive patient care
This self-awareness and willingness to refer patients when needed not only underscores the professionalism of NPs but also reinforces their commitment to patient well-being. It's a critical factor in maintaining trust within the healthcare system and ensuring that patients receive the most appropriate care for their specific needs.
The American Association of Nurse Practitioners emphasizes the importance of this collaborative approach. While full practice authority allows NPs to provide a wide range of services independently, it doesn't mean working in isolation. Instead, it enables NPs to practice to the full extent of their education and training while recognizing when specialist intervention is required.
This respect for professional boundaries also extends to complex cases and emergency situations. In emergency departments or when dealing with intricate medical issues, NPs often work closely with physicians, each bringing their unique skills to the table. This teamwork approach ensures that patients benefit from a comprehensive range of expertise.
By focusing on areas within their scope of practice and making judicious referrals, nurse practitioners effectively complement the services provided by physicians. This collaborative model of care helps address the physician shortage, and enhances the overall quality of healthcare delivery, creating a more robust and responsive system for all patients.
Full Practice Authority: A Key to Alleviating the Physician Shortage
While respecting professional boundaries is crucial, expanding the scope of practice for nurse practitioners (NPs)through Full Practice Authority (FPA) could be a pivotal solution to the worsening physician shortage. FPA allows NPs to evaluate patients, diagnose, interpret diagnostic tests, and prescribe medications without mandated physician supervision or collaboration.
As of 2025, 34 states and the District of Columbia have granted Full Practice Authority—up from just 22 in 2020. States like Texas, Tennessee, Michigan, and South Carolina are among the latest to pass FPA laws, reflecting bipartisan recognition of the vital role nonphysician practitioners play in primary care access and cost containment.
Advocates of FPA argue that empowering NPs helps close care gaps caused by the shortage of primary care physicians, especially in rural and underserved areas. And they’re not wrong—research shows rural counties in FPA states are 62% more likely to have at least one NP providing primary care services compared to similar counties in restricted states.
A recent systematic review in the Journal of the American Medical Association (2023) found that removing NP practice restrictions is linked to better healthcare access, without compromising patient outcomes. That’s a big win for patients, especially those managing chronic conditions or needing preventive care.
Further supporting this shift, recent research found that in designated Health Professional Shortage Areas (HPSAs), the number of NPs and PAs jumped from 72,000 in 2011 to 110,000 in 2023, while the number of physicians remained stagnant.
This reinforces that expanding NP autonomy through Full Practice Authority isn't about replacing physicians—it’s about reinforcing the healthcare team where it's needed most.
The benefits of Full Practice Authority include:
- Increased access to primary care services in underserved communities
- Cost-effective care delivery, with FPA states reporting an 11% reduction in primary care costs
- Shorter wait times—average patient wait dropped by 8 days within 2 years of FPA adoption
- Improved outcomes—hospitalizations for chronic conditions fell by 7–12% in areas with high NP utilization
- Higher NP satisfaction and pay—NPs in FPA states earn 12–15% more on average
While physicians remain essential for complex cases and specialized treatments, FPA allows the healthcare team to function more efficiently. Nurse practitioners and physician assistants can manage a significant portion of care independently, freeing up physicians for higher-acuity needs.
The takeaway? Full Practice Authority doesn’t replace physicians—it relieves them. It ensures patients get timely, high-quality care from the right provider at the right time. And in a system strained by workforce shortages and rising costs, that’s exactly the kind of solution we need.
Patient Outcomes: The True Measure of Nurse Practitioner Effectiveness
While Full Practice Authority can expand access to care, the real test of its success—and indeed, the success of nurse practitioners in general—lies in patient outcomes. This is where NPs have consistently demonstrated their value to the healthcare system.
Numerous studies have highlighted the effectiveness of nurse practitioners in delivering high-quality patient care. The evidence shows that NPs not only match physician-led care in many areas but can also lead to improvements in several key healthcare metrics:
- Reduced hospital readmission rates: NPs have been successful in providing follow-up care that prevents unnecessary rehospitalizations.
- Decreased hospitalizations from nursing homes: NP-led care in long-term care facilities has shown to reduce the need for hospital transfers.
- Improved overall health outcomes: By focusing on preventive care and chronic disease management, NPs help reduce preventable hospitalizations.
- Enhanced patient satisfaction: Many patients report high levels of satisfaction with NP-led care, citing factors such as thorough explanations and ample time for consultations.
- Cost-effective care delivery: NPs often provide comparable care to physicians at a lower cost, contributing to overall healthcare system efficiency.
These positive outcomes are, of course, predicated on NPs operating within the bounds of their training and making appropriate referrals when necessary. This aligns with the earlier discussion on professional boundaries and the importance of collaborative care.
It's crucial to recognize that patient outcomes should be the ultimate yardstick for assessing the role and contributions of nurse practitioners in the healthcare system. As the debate continues over why nurse practitioners are increasingly taking on roles traditionally held by doctors, these outcome measures provide compelling evidence of their effectiveness.
Conclusion: Nurse Practitioners – Augmenting, Not Replacing, Physicians
The question, "Why are nurse practitioners replacing doctors?" misses the mark. In reality, NPs enhance and complement physician care, not replacing it entirely.
By 2023, more than 280,000 nurse practitioners were delivering care across hospitals, clinics, emergency rooms, and underserved communities.
Together with physician assistants, they now make up roughly one-third of the nation’s clinical workforce. In areas hit hardest by provider shortages, the number of these nonphysician practitioners surged, rising from 72,000 to 110,000 in Health Professional Shortage Areas over the last decade, while physician counts stayed flat.
This isn’t about replacement it’s about reinforcement. When smartly integrated, these roles expand access, relieve overburdened systems, and make care more equitable and Nurse practitioners play a crucial role in our evolving healthcare landscape:
- Addressing the physician shortage: NPs help fill critical gaps, especially in primary care and underserved areas.
- Cost-effective care: NPs provide quality care at lower costs, helping to manage rising healthcare expenses.
- Improved access: With Full Practice Authority, NPs can offer a wider range of services, increasing healthcare accessibility.
- Positive patient outcomes: Studies show NPs deliver care that often matches or exceeds physician-led care in many primary care scenarios.
However, NPs cannot fully replace physicians due to differences in training and scope of practice. Complex cases and specialized care remain firmly in the physician's domain.
The optimal solution lies in a collaborative model:
- NPs manage a significant portion of primary and preventive care.
- Physicians focus on complex diagnoses and specialized treatments.
- Patients benefit from improved access, potentially shorter wait times, and comprehensive care.
This approach doesn't replace physicians but strategically distributes healthcare resources to meet growing patient needs. By embracing the unique strengths of both NPs and physicians, we can create a more robust, accessible, and efficient healthcare system.
The future of healthcare isn't about NPs replacing doctors. It's about fostering a collaborative environment where all healthcare professionals work together to provide the best possible patient care. This evolution in healthcare delivery promises to improve access, reduce costs, and ultimately lead to better health outcomes for all.
Find a preceptor who cares with NPHub
Book a rotation.webp)








.webp)


.webp)


%20(3)%20(2).svg)
.webp)