Did you know there are over 355,000 Nurse Practitioners (NPs) licensed in the U.S.? And guess what? The healthcare industry is finally catching on to just how essential NPs are.
Why? Because NPs play a massive part in how we experience healthcare today.
From improving access to care to championing evidence-based practices, NPs are making an undeniable impact on patient outcomes every single day. If you’ve ever wondered just how much NPs are changing the game, you’re in the right place.
Lets talk about three powerful ways NPs drive better health outcomes, proving once again why they’re the backbone of patient-centered care.

1. Providing quality services equivalent to Physicians to improve patient outcomes
Nurse Practitioners (NPs) are delivering care that matches, and in some cases, exceeds the quality of physician-led treatment. Their ability to provide comprehensive, patient-centered care has been backed by research, showing their role is not just essential but highly effective in improving patient outcomes and clinical outcomes.
Here’s what evidence based practice tells us about the value NPs bring to patient care:
- Consistency in Patient Outcomes: A 2004 study by Lenz et al. found no significant difference in quality care or satisfaction between patients treated by NPs and physicians. It is also worth noting that patients treated by physicians had a higher average primary care utilization than those treated by NPs.
- Cost-Effective Care: Liu et al. (2020) discovered that patients assigned to NPs were less likely to use primary care, specialty care, and inpatient services. Yet, when it came to costs and managing chronic diseases, NP-treated patients fared just as well as those treated by MDs.
- Reliability & High Standards: The Office of Technology Assessment affirms that NPs match doctors in critical patient outcomes, such as survival rates and satisfaction levels. This stamps their reliability as top-tier healthcare providers..
Beyond these key findings, research by Maung Htaya and Dean Whitehead also highlights additional advantages:
- Patients reported higher satisfaction with NP consultations compared to general practitioners.
- NP consultations lasted longer on average (12.2 minutes vs. 9.2 minutes for GPs), allowing for more thorough assessments and patient education.
- Patients felt they received better communication, including clearer explanations about their conditions and treatment plans.
- More patients expressed willingness to seek same-day appointments with NPs in the future.
- NPs contributed to a significant reduction in waiting times, improving overall access to care.
- NPs have been shown to significantly reduce the incidence of hospital acquired infections through diligent monitoring and evidence-based practices.
NPs provide both medical treatment while they take a holistic approach, addressing the full scope of a patient’s health concerns. Their ability to integrate evidence-based practice into patient care leads to better outcomes, fewer complications, and more efficient recovery times.
As the demand for quality healthcare grows, NPs are proving to be indispensable in delivering high-level, accessible, and patient-focused care.

2. Keeping Healthcare costs lower
Nurse Practitioners (NPs) are not only providing top-tier healthcare but also helping to make health systems more financially sustainable. Their ability to deliver high-quality care at a lower cost makes them essential in today’s healthcare system, where expenses continue to rise.
Significant cost savings without compromising care
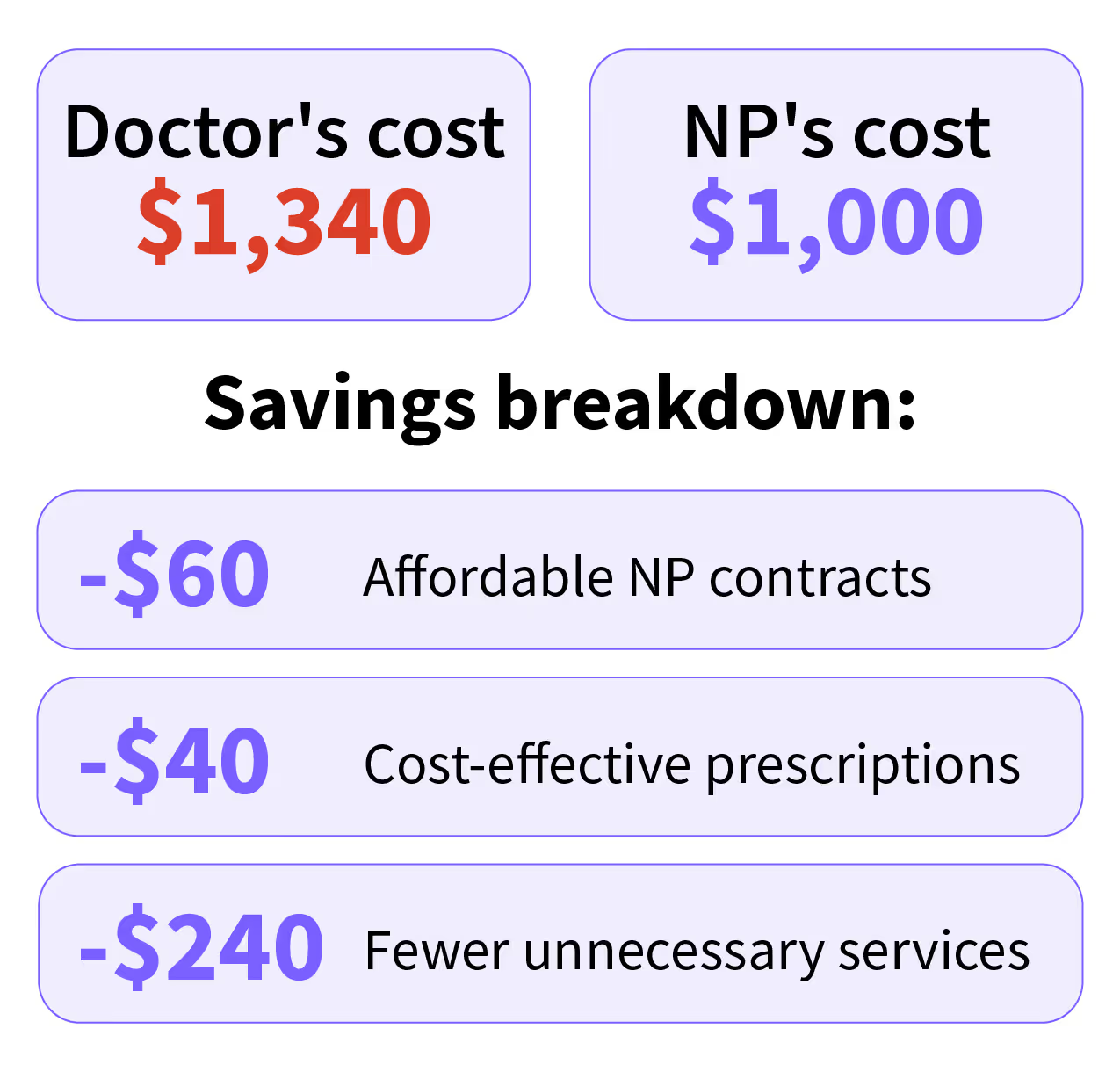
Research shows that healthcare organizations can reduce costs by up to 34% when utilizing NPs compared to physician-led care, with a 21% reduction for high-risk patients. These savings stem from:
- Lower consultation costs while maintaining high-quality treatment
- Reduced hospital admissions due to effective chronic disease management
- Decreased reliance on specialty and emergency care through early intervention and preventive strategies
NPs are skilled in tailoring treatment to individual patient needs, ensuring that necessary care is delivered efficiently without unnecessary expenses.
Here’s an example breakdown for a low-risk patient to help you understand the savings:
Expanding access and reducing financial barriers
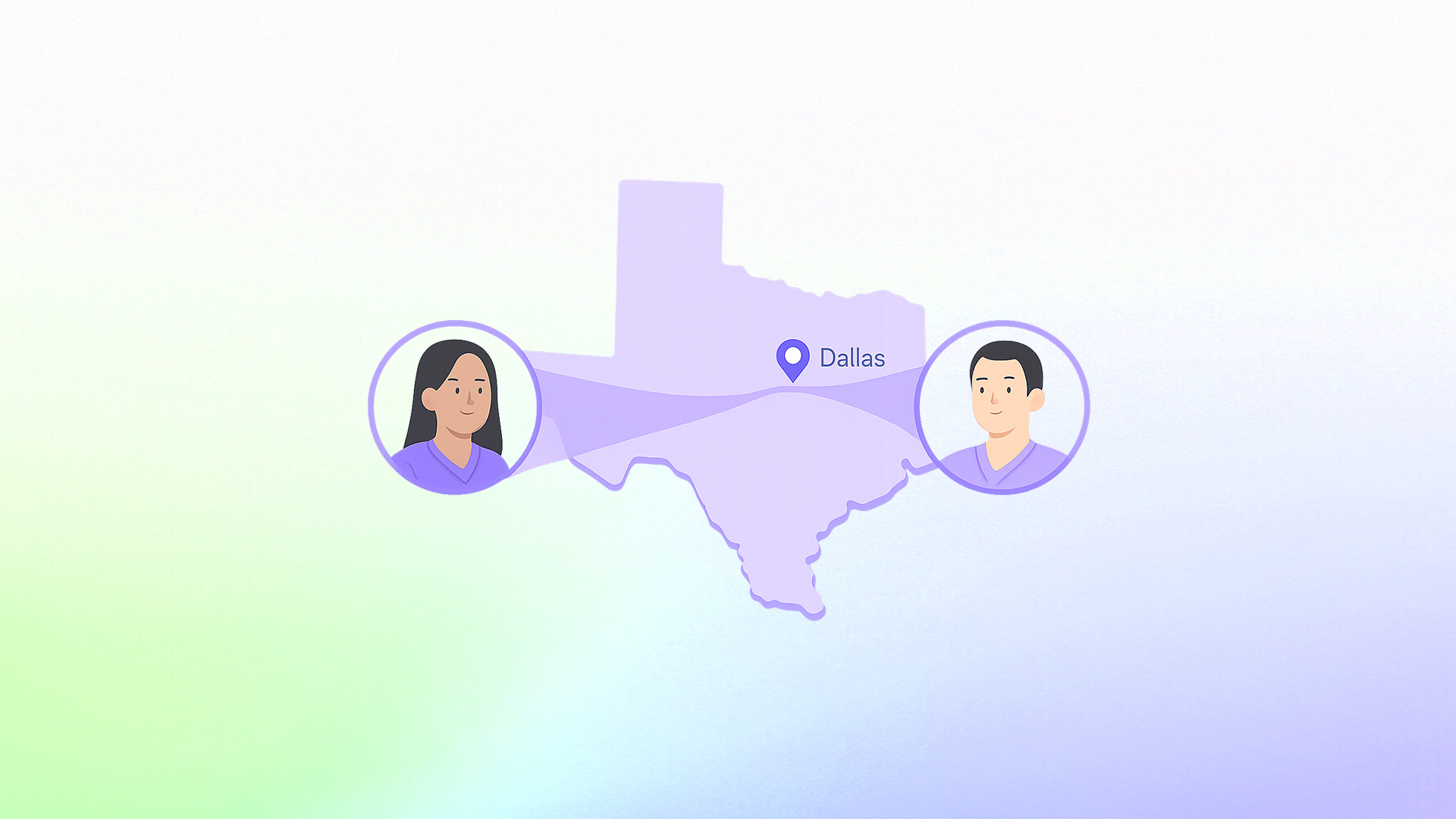
In many underserved areas, patients must travel 30 miles or more to access medical facilities. NPs help close these gaps by providing localized, community-based care, ensuring timely and effective treatment to enhance patient outcomes.
Beyond direct cost savings, NP-driven care leads to:
- Shorter wait times for appointments and urgent care
- Longer, more thorough consultations compared to traditional primary care models
- Higher patient satisfaction due to improved communication and holistic care approaches
A financially sustainable healthcare model
At a systems level, NP-led models offer long-term financial benefits, including:
- More efficient use of healthcare resources, reducing the strain on hospitals and specialists
- Alternative funding models that support NP-centric care without over-reliance on physician-dominated systems
- A greater focus on prevention and chronic disease management, which lowers long-term healthcare costs
When NPs operate at the top of their scope, they bridge the gap between cost-efficiency and high-quality care, making healthcare more accessible and sustainable. By integrating innovative service delivery models, NPs are proving that healthcare can be both affordable and effective—without sacrificing patient outcomes.

3. Expanding the reach and efficiency of Physician practices
Nurse Practitioners (NPs) play a crucial role in enhancing healthcare efficiency while maintaining high-quality patient care. By seamlessly integrating into medical teams, they expand patient capacity, reduce delays, and improve overall healthcare outcomes, leading to better patient outcomes.
Optimizing workflows and reducing Physician burden
With growing patient demands, long wait times, and physician shortages, healthcare systems need solutions that increase efficiency without sacrificing quality. NPs are proving to be that solution. Studies show that NPs:
- Improve patient flow, ensuring quicker assessments and timely discharges in acute care settings
- Reduce the workload of overburdened medical staff, allowing physicians to focus on more complex cases
- Lower hospital readmission rates by managing chronic conditions and providing thorough follow-up care
By handling a wide range of primary and specialty care services, NPs allow physicians to focus on high-acuity patients, ensuring that all individuals receive the appropriate level of care. This division of labor benefits both patients and providers—patients experience shorter wait times, and physicians avoid burnout.
Reducing hospitalizations and strengthening preventive care
NPs are also key players in reducing preventable hospitalizations and emergency department visits. Their presence in nursing homes and outpatient settings has led to:
- Fewer hospitalizations from nursing facilities, as NPs effectively manage chronic illnesses on-site
- A decrease in unnecessary hospital admissions, through proactive and preventive care approaches
- Improved patient outcomes by emphasizing disease prevention, early intervention, and holistic care, ultimately improving health outcomes
These contributions not only improve patient experiences but also create a more financially sustainable healthcare system. By preventing complications before they escalate, NPs help cut down overall healthcare expenditures while enhancing patient health.
Shaping a more accessible and patient-centered system
The role of NPs extends beyond efficiency—they are also champions of patient-centered care. Their approach prioritizes:
- Longer, more personalized consultations, allowing for better communication and patient understanding
- A whole-person wellness model, addressing both medical and lifestyle factors that impact health
- More accessible healthcare, particularly in underserved communities where physician shortages are prevalent
By balancing cost, quality, and accessibility, NPs are reshaping the healthcare system. Their expanding influence marks a shift toward a more efficient, patient-focused model—one where healthcare is not just about treating diseases, but about sustaining long-term wellness and equity in care.
As demand for effective and affordable healthcare grows, the role of Nurse Practitioners will continue to be a driving force in revolutionizing the industry—proving that better care doesn’t always have to come at a higher cost.

4. Encouraging preventative care: The Nurse Practitioner’s role in long-term health
Preventative care is one of the most effective ways to reduce disease burden, lower healthcare costs, and improve overall public health. Nurse Practitioners (NPs) are at the forefront of this movement, promoting early detection, lifestyle changes, and patient education to keep individuals healthier for longer.
Empowering patients through education
NPs play a critical role in health promotion by educating patients on lifestyle choices that prevent chronic conditions. Their approach goes beyond treatment—it focuses on prevention, ensuring that patients understand:
- The importance of routine screenings for conditions like diabetes, hypertension, and cancer
- How nutrition, physical activity, and stress management contribute to long-term health
- The impact of lifestyle choices on chronic disease development and progression
By incorporating education into every patient interaction, NPs encourage proactive health management and help individuals make informed decisions about their well-being.
Chronic disease prevention and early screening
Chronic diseases—such as diabetes, cardiovascular conditions, and mental health disorders—are among the leading causes of death and disability. NPs play a crucial role in both early detection and long-term management, ensuring that patients receive:
- Regular screenings to identify health risks before they become serious
- Personalized management plans to prevent complications
- Ongoing monitoring to adjust care based on patient needs
By focusing on early intervention, NPs help reduce hospital admissions and prevent unnecessary complications, ultimately improving patient quality of life.
Expanding access to preventative care
In many underserved areas, access to preventive services is limited—but NPs are bridging this gap. By providing community-based care, NPs:
- Ensure rural and low-income populations receive regular check-ups and preventative services
- Offer flexible care models, such as telehealth and mobile clinics, to reach more patients
- Provide consistent, patient-centered care, which fosters trust and encourages people to seek care earlier
Through their presence in clinics, schools, and community health centers, NPs ensure that preventative care is not just available but accessible to those who need it most.
Advocating for preventative care in healthcare policy
NPs are not only frontline providers but also policy advocates for preventative care integration into the healthcare system, utilizing healthcare research to support their efforts. Their efforts include:
- Supporting legislative changes that expand NP scope of practice for preventative services
- Advocating for insurance coverage of routine screenings and wellness visits
- Promoting public health initiatives that encourage disease prevention and early detection
Through these efforts, NPs help shift the healthcare system from reactive to proactive, ensuring that prevention becomes a cornerstone of primary care.
Collaborating for holistic, preventative healthcare
Preventative care doesn’t stop at medical treatment—it requires a multidisciplinary approach. NPs work alongside:
- Dietitians and fitness specialists to develop sustainable health plans
- Mental health professionals to address behavioral factors affecting physical health
- Community organizations to connect patients with resources that support long-term wellness
By integrating medical, behavioral, and social determinants of health, NPs provide holistic, patient-centered care that promotes long-term well-being.
A Stronger role for NPs in positive patient outcomes
As healthcare continues to shift toward patient-centered, prevention-based models, Nurse Practitioners are proving to be indispensable in delivering high-quality, cost-effective care.
Their impact goes far beyond treating illness, NPs are actively shaping the future of healthcare by improving access, advocating for policy change, and emphasizing patient safety and long-term wellness over reactive treatment.
By integrating education, early intervention, and holistic care into their practice, NPs are not redefining how healthcare is delivered.
Their presence in both primary and specialized care settings ensures that more patients receive timely, evidence-based treatment, reducing preventable hospitalizations and improving overall outcomes.
The healthcare landscape is changing, and NPs are at the center of this transformation. Their ability to balance quality, affordability, and accessibility makes them a driving force in building a system that prioritizes prevention, efficiency, and whole-person care.
As their influence continues to grow, it is clear that the future of healthcare is not just about treating disease it is about creating a healthier population through proactive, patient-focused solutions led by Nurse Practitioners.
Frequently Asked Questions:
What is the role of a Nurse Practitioner in a healthcare setting?
Nurse Practitioners (NPs) are highly trained healthcare providers who bridge the gap between nursing and medicine. With advanced education and clinical training, they diagnose and treat illnesses, prescribe medications, and manage patient care with a holistic approach. Their focus on evidence-based practice improves patient outcomes, enhances healthcare efficiency, and promotes preventative care. Additionally, NPs play a critical role in patient education, empowering individuals to take charge of their health and adhere to treatment plans.
Can a Nurse Practitioner provide care of equal quality to a physician?
Yes, and research consistently supports this. Numerous studies have shown that NPs deliver healthcare services with comparable patient outcomes to physicians, including in areas such as chronic disease management, preventive care, and patient satisfaction. In fact, patients often report higher levels of communication and longer consultation timeswith NPs, leading to improved understanding and adherence to treatment.
How do Nurse Practitioners expand the reach of physician practices?
NPs play a vital role in increasing efficiency and patient access within physician-led practices. By managing routine care, chronic conditions, and preventive screenings, they allow physicians to focus on more complex cases. Their involvement helps reduce unnecessary emergency visits, lower hospital readmission rates, and streamline patient flow, ultimately making healthcare more accessible and effective.
What role do Nurse Practitioners play in preventative care?
Preventative care is a cornerstone of NP practice. By promoting regular screenings, educating patients on healthy lifestyles, and managing chronic diseases early, NPs help prevent more serious health complications down the line. Their proactive approach reduces healthcare costs, enhances long-term patient well-being, and ensures earlier intervention for at-risk populations.
Where do Nurse Practitioners make the biggest impact?
NPs significantly impact underserved and rural communities, where physician shortages often limit access to care. They also excel in primary care, geriatrics, mental health, and chronic disease management, areas where patient education and long-term care coordination are crucial. Their ability to deliver comprehensive, cost-effective, and patient-centered care continues to transform the healthcare landscape.
Find a preceptor who cares with NPHub
Book a rotation.webp)







.webp)

.webp)


.webp)